Pertussis
Key facts
-
Pertussis (whooping cough) irritates the airways (makes them sore or painful), which causes long coughing fits that can be very severe.
-
Small babies can die from pertussis (whooping cough).
-
Vaccines are the best way to protect your child against pertussis (whooping cough).
On this page
- What is pertussis (whooping cough)?
- What will happen to my child if they catch pertussis (whooping cough)?
- What vaccine will protect my child against pertussis (whooping cough)?
- When should my child be vaccinated?
- How does the pertussis (whooping cough) vaccine work?
- How effective is the vaccine?
- Will my child catch pertussis (whooping cough) from the vaccine?
- What are the common reactions to the vaccine?
- Are there any rare and/or serious side effects to the vaccine?
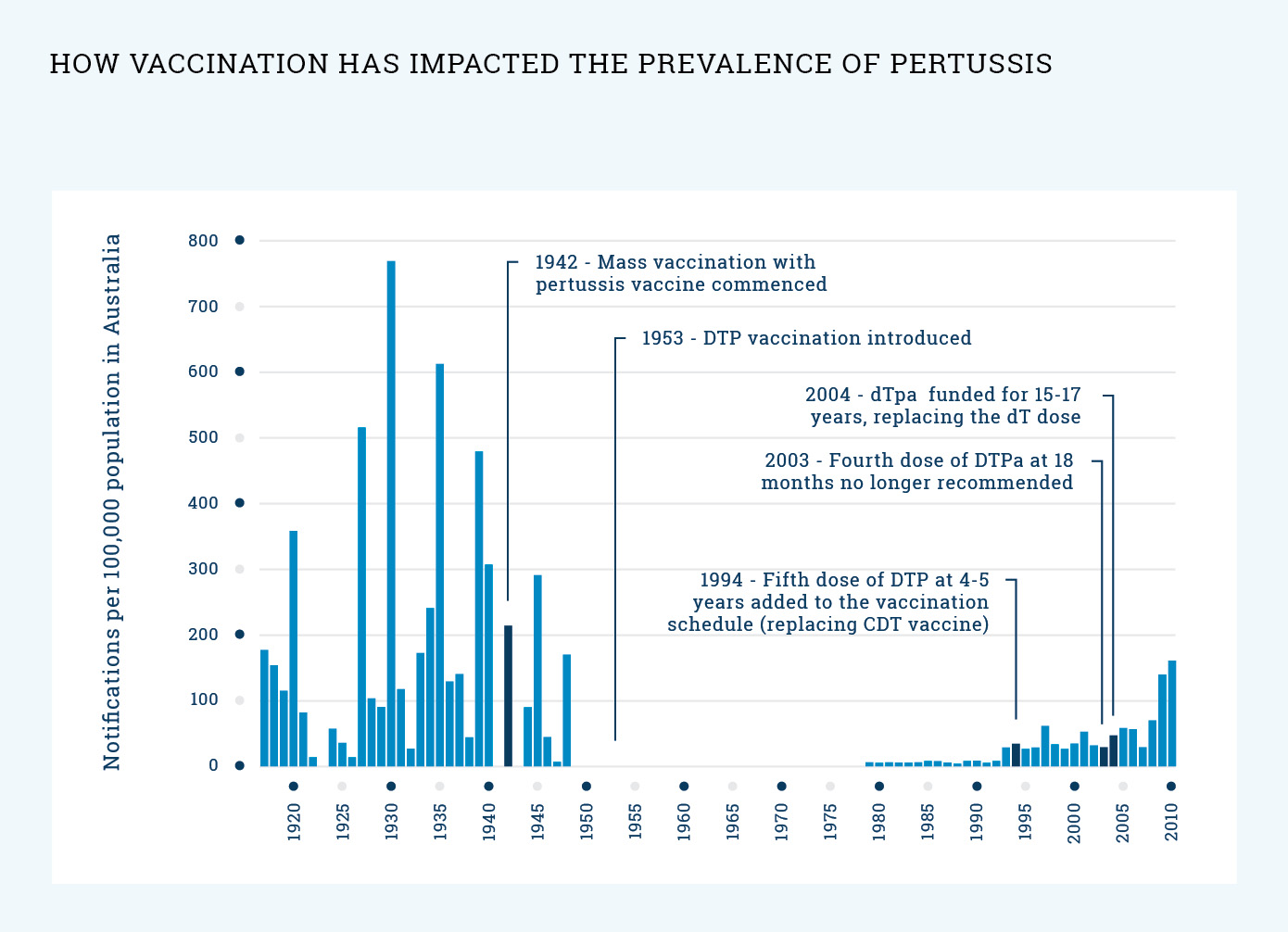
- What impact has vaccination had on the prevalence of pertussis (whooping cough)?