Diphtheria
Key facts
-
Diphtheria is a serious disease that can cause breathing difficulties; heart, brain and nerve damage; and, in some cases, death.
-
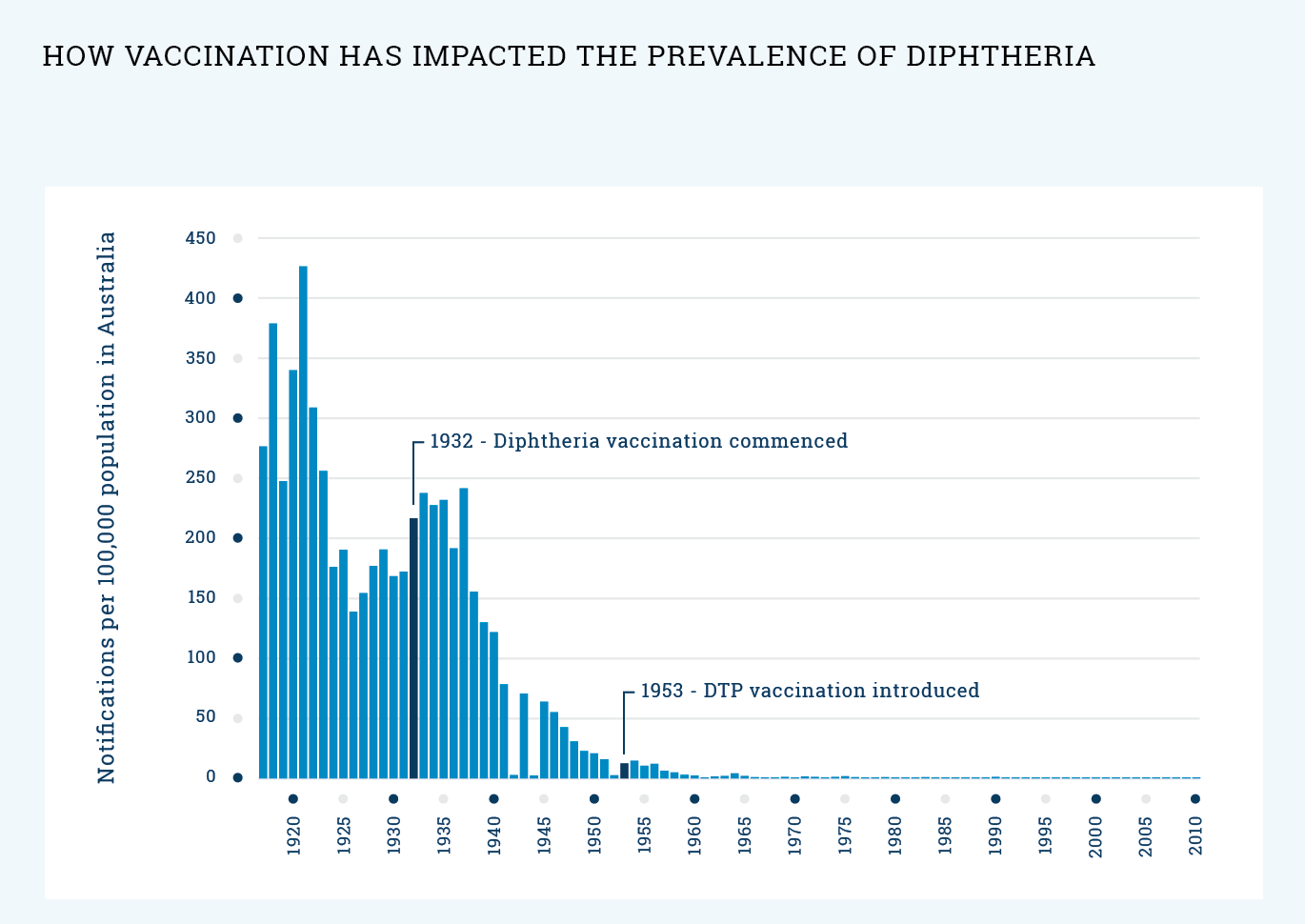
Due to the vaccination program, diphtheria has been rare in Australia for a long time, but recently a small number of cases have been reported again.
-
In Australia, all infants and young children are recommended to be vaccinated against diphtheria. To keep this level of protection in adolescence, a booster dose is recommended for all 12- and 13-year-olds.
On this page
- What is diphtheria?
- What will happen to my adolescent if they catch diphtheria?
- What vaccine will protect my adolescent against diphtheria?
- When should my adolescent be vaccinated?
- How does the diphtheria vaccine work?
- How effective is the diphtheria vaccine?
- Will my adolescent catch diphtheria from the vaccine?
- What are the common reactions to the vaccine?
- Are there any rare and/or serious side effects to the vaccine?
- What impact has vaccination had on the spread of diphtheria?
- What if I still have questions?