Meningococcal disease
Key facts
-
Meningococcal disease can cause swelling around the brain (meningitis) and blood poisoning (bacteria in the blood – also called septicaemia).
-
It is recommended that your adolescent receives vaccines that protect them against different types (strains) of meningococcal disease. This includes one vaccine dose to protect against four strains of meningococcal disease (A, C, W and Y) and two vaccine doses to protect against meningococcal B.
-
Vaccines are the best way to protect your adolescent against meningococcal disease.
On this page
- What is meningococcal disease?
- What will happen to my adolescent if they catch meningococcal disease?
- What vaccine will protect my adolescent against meningococcal disease?
- How do vaccines work?
- How effective are vaccines?
- When should my adolescent be vaccinated?
- Will my adolescent catch meningococcal disease from the vaccine?
- What are the common reactions to the vaccine?
- Are there any rare and/or serious side effects to the vaccine?
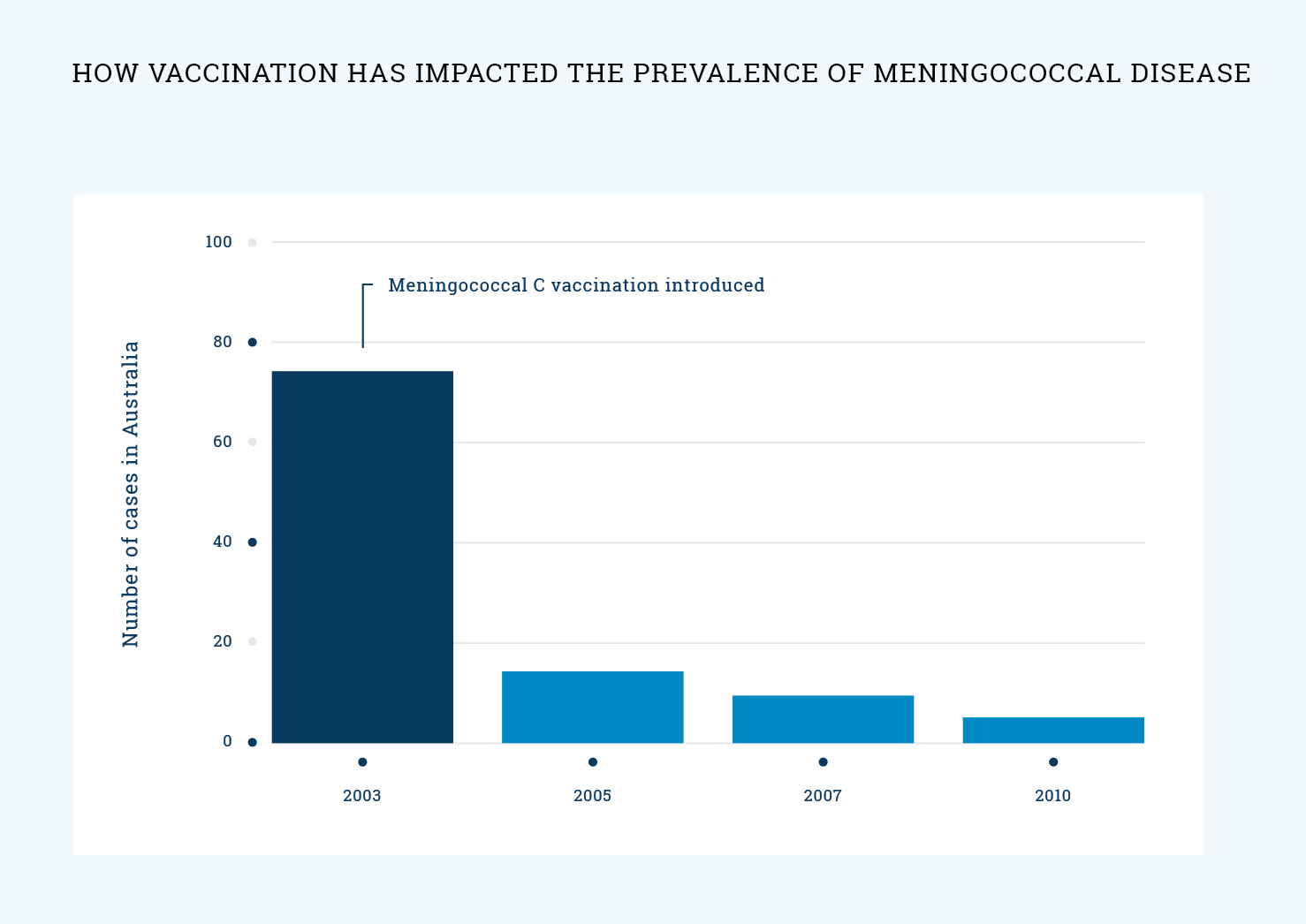
- What impact has vaccination had on the spread of meningococcal disease?
- What if I still have questions?